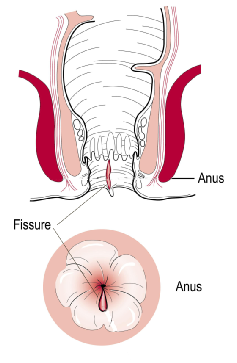
Anal Fissure
An anal fissure is a visible tear in the lining of the anal canal that extends from the skin on the outside of the anus inwards for a variable distance. Anal fissures occur in one in every 300 people. They occur with equal frequency between men and women, and generally in people aged 15–40 years.
The classic symptoms are a sharp anal pain and bright red bleeding from the rectum when going to the toilet. These symptoms may or may not occur together. Some people merely have a mucus discharge. Surprisingly, some people with an anal fissure have no symptoms whatsoever. An anal fissure may sometimes be found incidentally on examination for other anal problems.
The tear or ulcer associated with an anal fissure is generally closed when the anus is closed. When the anus opens during passing of a stool, underlying nerves are activated, triggering a sensation of pain.
There is great debate about the causes of uncomplicated anal fissures. Some people maintain that the passing of a hard stool can tear the lining of the anus, but in reality we are unsure. What is known is that in some people there is a relatively poor blood supply to the front and rear of the back passage and, for whatever reason, an ulcer may form. The anal muscle may go into spasm, with a further reduction in this poor blood supply, impairing healing of the ulcer. When healing does occur, this is of poor quality and the skin easily breaks down again. There are other conditions in which a fissure can form, but in association with a weak anal sphincter; these people generally do not have a poor blood supply to the area.
A number of medical conditions are associated with anal fissures. They are very common during pregnancy and after childbirth. Inflammatory bowel disease can lead to unusual types of anal fissures that are very difficult to manage. Sometimes, an anal fissure can indicate the presence of a sexually transmitted disease.
Most people only develop one fissure. This is usually at the rear of the anal canal (one in 10 people develop the fissure at the front). Occasionally people with an otherwise normal anal canal can develop fissures at both the front and rear of the anal canal, but in patients with atypical fissures and weak anal sphincter muscles, we expect to find another condition present, such as inflammatory bowel disease or an internal rectal prolapse.
Treatment
Medical
Conservative measures generally do not aid healing, but can lessen symptoms while the anal fissure is healing. Many fissures heal without treatment, especially in the first three months. Hot baths and salt baths do not help in any way. Stool softeners can help less the pain of going to the toilet.
Diltiazem cream applied twice daily for six weeks to the outside and if possible inside of the anus can help to relax the anal muscles and increase the blood supply to the area, which aids healing. The amount of relaxation is only slight, so does not interfere with bowel continence. Unfortunately, if the fissure has been present for over six months, treatment with diltiazem cream is only successful in three of 10 people.
Surgical
Surgery is considered if conservative measures or a course of diltiazem cream has failed.
Botulinum toxin injection into the anal sphincter is often tried first for a non-healing anal fissure. This relaxes the sphincter slightly, increases the blood supply, and may improve healing. If there is a significant scar associated with the anal fissure, this will need to be removed, which can make the procedure quite painful. Not all people have scarring, so this is not always necessary.
A rectal advancement flap or a lateral anal sphincterotomy may be also considered. The anus has an inner and outer set of circular muscles. A lateral sphincterotomy cuts a small portion of the inner set of muscles, making the anus more relaxed, improving the blood supply and promoting healing. Using the rectal advancement flap method, a piece of tissue with a good blood supply from the rectum or the skin outside into the anus is moved into the anus to cover the anal fissure. The success rate is around 95% for a lateral anal sphincterotomy and about 60% for a rectal advancement flap.
For more detailed information on anal fissures, please visit http://patient.info/health/anal-fissure

