Hernias
A hernia occurs when there is a weakness in the muscular abdominal wall that keeps the abdominal organs in place. This weak area allows organs and tissues to push through, or herniate, producing a bulge. The weakness may be present from birth or develop over a long period of time. Anything that increases the pressure in the abdomen can increase the risk of developing a hernia. Being overweight or obese, straining while moving or lifting heavy objects, having a persistent heavy cough, and having a history of multiple pregnancies are known risk factors for abdominal hernia. The risk of developing an abdominal hernia is increased in patients with certain medical conditions, such as emphysema, and those on dialysis for kidney disease.
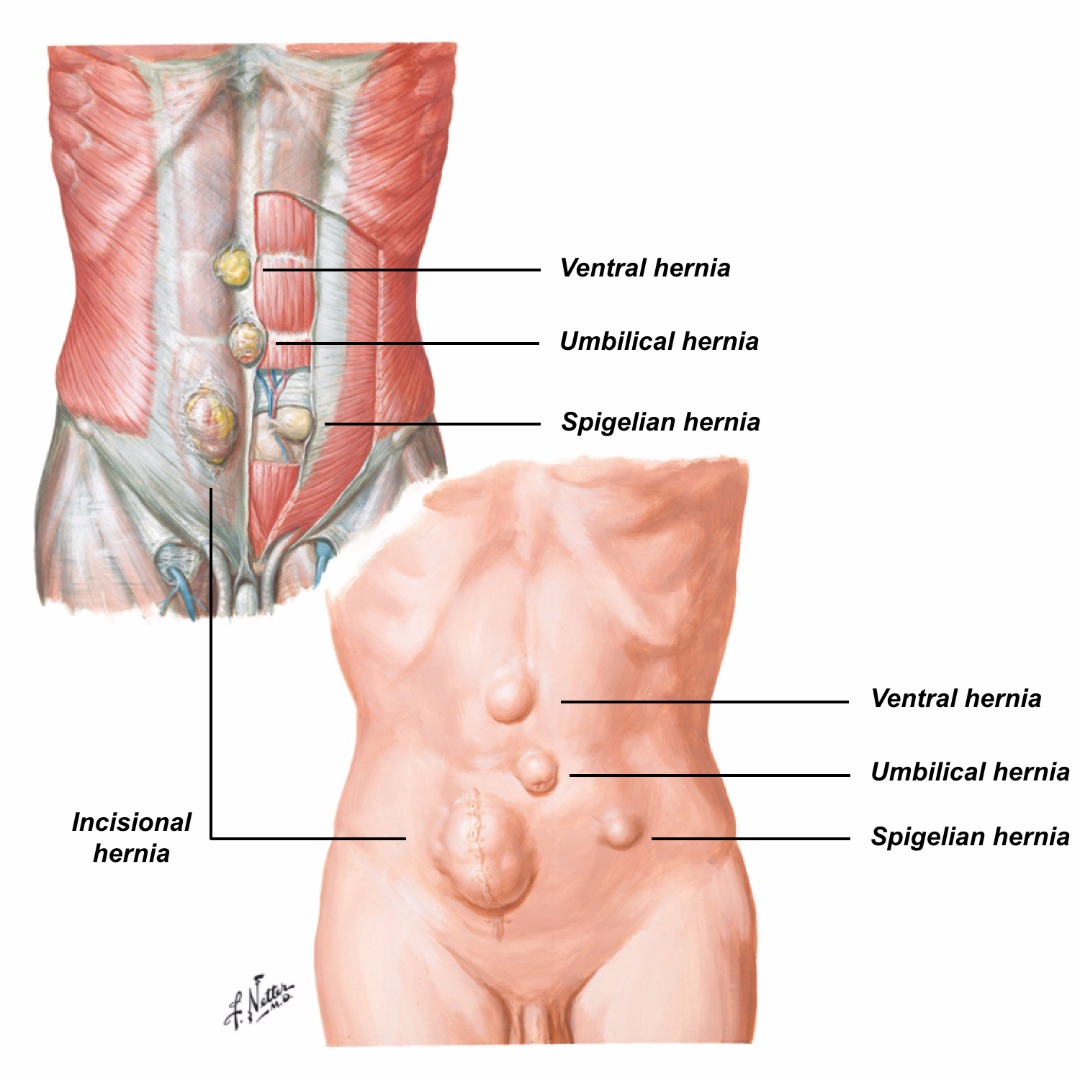
The four types of abdominal hernia commonly seen in a colorectal clinic are:
-
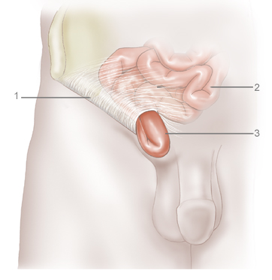
Inguinal hernia – a hernia occurring in the groin and found more often in men than in women. Inguinal hernia occurs in about 25% of men but in only 3% of women. They are more common in infants and in men aged older than 50 years.
-
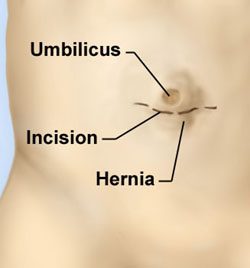
Umbilical hernia – this type of hernia occurs near the navel (belly button) and is common in infants and young children, especially in babies born prematurely. In many cases, the hernia disappears and the abdominal muscles reseal in the first few months of life, but a minority of children need surgery. An umbilical hernia can also develop in adults, who may have had a weak area around the navel since birth.
-
Femoral hernia – a rarer type of hernia, occurring mainly in women and accounting for 2% of all hernias and 6% of all groin hernias. The risk of developing a femoral hernia increases with age, so most of these hernias are found in middle-aged or older women. They are thought to be more common in women because of their wider pelvis and a slightly larger femoral canal, into which intestinal tissue can herniate more easily than in men. Femoral hernias can be easily confused with inguinal hernias by both patients and doctors.
-
Incisional hernia – a hernia that occurs through a previously made surgical incision in the abdomen. They are thought to be caused by failure of a surgical wound to heal, but are probably the result of multiple patient and technical factors. An incisional hernia is most likely to appear at around 6 weeks after surgery, when people become more physically active. Advances in surgical technique and materials have not removed this problem. Overall, the risk of developing an incisional hernia is about 1%, but may be up to 20% in patients with malnutrition, wound infection or diabetes, if the patient has been on corticosteroids, or if surgery is being performed as an emergency.
Symptoms
An abdominal hernia is felt as a lump in the groin (inguinal and femoral hernias), around the navel (umbilical hernia), or at the site of previous abdominal surgery (incisional hernia). People with an abdominal hernia may have no symptoms whatsoever and their hernia may only be found on examination by a doctor for something else. Some people do get pain from their hernia, especially when lifting. The hernia may appear to get bigger when laughing, coughing, or going to the toilet, and then shrink when the person is relaxing or lying down. Symptoms vary during the day. If the person has a strenuous job, any straining may increase the size of the hernia. The early small hernias seem to cause more symptoms. These symptoms may then diminish or go away altogether as the hernia gets slightly bigger, only to reappear when the hernia becomes even larger.
Diagnosis
An experienced colorectal surgeon can readily diagnose an abdominal hernia by taking a detailed history and performing a clinical examination. The hernia usually presents as a lump under the skin, which may only be present on standing up and disappear on lying down. Occasionally an abdominal hernia may be producing typical symptoms but be harder to find. In these cases, a CT scan or ultrasound may be useful.
Treatment
Conservative
If a hernia is small and causing no symptoms, it can be left safely alone initially. However, hernias don't go away of their own accord. Over time, hernias tend to get bigger as the abdominal wall gets weaker and more tissue bulges through. Still, many people are able to delay surgery for months or even years.
Some people have additional medical problems that increase the risks associated with surgery to the point that these risks are greater than the risk of leaving the hernia alone. The treatment recommended for these patients is usually a custom-made corset (truss) to provide support for the hernia.
Surgery
Surgery is recommended for most adults with an abdominal hernia as the hernia is unlikely to get better by itself and will almost certainly get worse over time. Further, the risk of complications increases with age. Any patient with increasing symptoms from a hernia, a hernia that is increasing in size and/or not getting smaller when lying down, or that is interfering with work performance or activities of everyday living should consider a surgical hernia repair.
If a hernia is not surgically repaired, there is a small but ever-present risk of the portion of bowel in the hernia becoming stuck (obstructed), causing intense pain and needing emergency surgery. There is also a risk of the portion of bowel lodged in the hernia losing its blood supply (becoming strangulated). A strangulated hernia is potentially fatal and requires emergency surgery within hours to release the trapped tissue and restore its blood supply. Emergency surgery in these circumstances may also require the affected part of the bowel to be removed.
The risks of obstruction and strangulation are much higher for femoral hernias, even small ones, than for the more common inguinal and umbilical hernias. If a femoral hernia is suspected (or cannot be excluded), an appointment with a colorectal surgeon should be made as soon as possible. Unfortunately, over half of patients with a femoral hernia still arrive in hospital as an emergency, with all the increased risks that entails.
Inguinal hernia repair, umbilical hernia repair, and femoral hernia repair can be performed by an open approach or a laparoscopic approach. Small and medium-sized hernias, especially if they are on both sides of the body, are usually best suited for a laparoscopic approach. Laparoscopic surgery is said to have a shorter recovery period. Larger hernias and hernias that are not reducing are often repaired by an open approach. The general recommendation is to use mesh for hernia repair as it markedly reduces the chances of the hernia coming back.
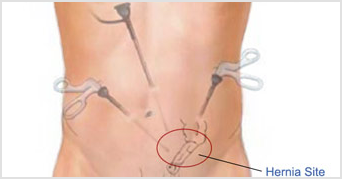
Open surgery and laparoscopic surgery are excellent procedures, but both have a 1% chance of the hernia returning. If a hernia recurs after a previous repair, the new repair may be best done using a different approach to that done previously. For example, if the previous hernia surgery that failed was an open repair, then laparoscopic surgery should be considered and vice versa. Laparoscopic surgery should probably not be performed in patients who have had major abdominal surgery before.
The pros and cons of abdominal hernia repair will be discussed in detail with you in advance of your surgery. For more detailed information on the more common types of abdominal hernia, please visit http://www.britishherniasociety.org/

