Haemorrhoids
The anus contains a cushion-like ring of blood vessels that, together with the sphincter muscles, have an important role in maintaining continence. When these vascular cushions, also known as haemorrhoid tissue, become enlarged and swollen, they are known as haemorrhoids (or “piles”).
Haemorrhoids are sometimes described as “varicose veins of the anus”. Varicose veins originate as normal veins, but, for a variety of reasons, can become bigger and cause symptoms. In a similar way, the vascular cushions in the anus are a normal body structure that can also become enlarged and cause symptoms.
Symptomatic haemorrhoids can occur in both men and woman and at any age. Generally speaking, they are most common in people aged 40–60 years. If you look closely enough, nine in 10 people will have haemorrhoidal disease, but most do not have significant symptoms. Overall, half the people with haemorrhoids will have trouble with them in their lifetime.
Many people believe that a diet low in fibre and fluid causing constipation is the main cause of haemorrhoids. However, the exact cause of symptomatic haemorrhoids is unclear. Diet and fluid clearly have a role, as does constipation, although there are people with chronic diarrhoea who suffer from haemorrhoids. Being overweight, having a chronic cough, or suffering from pelvic floor problems can also cause haemorrhoids. Genetics may also be involved. In some people there is no obvious cause.
Pregnant women are particularly prone to haemorrhoids because the growing foetus increases the pressure in the abdomen and hormonal changes cause the blood vessels within the haemorrhoid tissues to increase in size. Labour itself further increases the pressure on the haemorrhoid tissues.
Many patients feel guilty about developing haemorrhoidal disease. However, although a number of people could improve their haemorrhoids by changing their lifestyle and diet, many have done absolutely nothing wrong, and simple measures will not improve their symptoms.
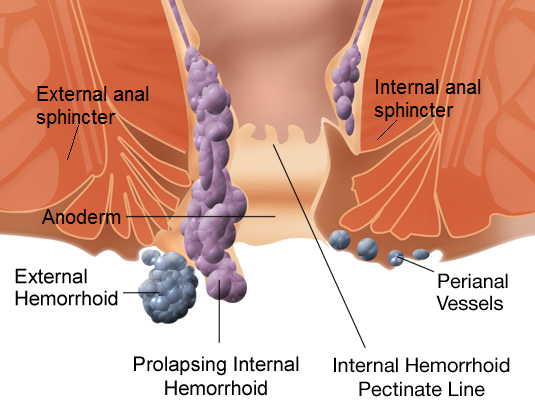
Colorectal surgeons define haemorrhoids as being internal or external. Internal haemorrhoids are those that form above a point 2–3 cm inside the anus in the upper part of the anal canal and receive a blood supply that comes downwards from the bowel. External hemorrhoids are usually found beneath the skin around the anal opening and receive a blood supply that comes upwards from the surrounding skin. The different blood supply for internal and external haemorrhoids explains why the treatment needed for the two types is different.
Both external and internal haemorrhoids can grow bigger, and internal haemorrhoids can become so large that they can fall out of place and protrude outside the anus. These are known as prolapsing internal hemorrhoids. External hemorrhoids are already outside the anus, so cannot prolapse. External hemorrhoids are easily confused with the more commonly found benign skin growths known as skin tags.
Most people with haemorrhoidal disease have no or very few symptoms. If symptoms do occur, they include bright red bleeding, mucus discharge, itching of the skin in and around the anal area, and prolapse of internal haemorrhoids. Often there is only mild discomfort, but pain can occur with haemorrhoids, particularly if a blood clot forms inside an external or prolapsed internal haemorrhoid. This is known as a thrombosed haemorrhoid, which can be extremely painful, especially for the first few days. Another condition known as a thrombosed perianal haematoma is easily confused with a thrombosed external haemorrhoid.
It is widely believed that any symptoms around the back passage must be from haemorrhoidal disease. This is far from the truth, and similar symptoms can arise from a wide range of conditions that involve the back passage, so should always be checked out.
Diagnosis
Haemorrhoids are diagnosed by physical examination. External haemorrhoids and skin tags can be diagnosed by simply looking at the skin surrounding the anus. A digital (finger) examination of the anal canal is then performed. A common misconception is that internal haemorrhoids can be felt by a finger – this is not the case because they only contain blood and the examining finger will compress them.
The only way to diagnose internal piles is by examining the anal canal with a narrow, hollow short tube known as a proctoscope. The proctoscope is inserted into the back passage and allows the colorectal specialist to see if haemorrhoids are present. When the proctoscope is being withdrawn, any internal haemorrhoids that are prolapsing out can be seen as well. This examination is not usually painful. It helps to exclude any other potentially serious causes for your symptoms, does not require anaesthesia, and can be done in the clinic.
The most common reason that people with symptoms affecting the back passage visit a colorectal specialist is to exclude bowel cancer. This is also in the back of the surgeon’s mind, so further tests may be ordered to look at the large bowel more closely. These tests may involve inserting a flexible telescope through the back passage to look at the large bowel or a computed tomography (CT) scan. These procedures are not done in the clinic, and will only be requested if necessary.
Treatment
Conservative
Thankfully, treatment is not usually required for haemorrhoidal disease. Many people, when reassured that nothing serious is going on, are happy to live with minor symptoms and bleeding. This is entirely safe. Most people with minor haemorrhoidal disease have intermittent symptoms that they learn to manage themselves. The mere presence of haemorrhoidal disease on examination does not mean treatment is needed. Leaving haemorrhoids untreated rarely causes any long-term problems. Haemorrhoids do not progress to cancer and hardly ever cause anaemia, despite significant blood loss. They can be safely left alone if the patient chooses.
Many patients benefit from increasing the fibre in their diet, decreasing their tea and coffee intake, and avoiding diarrhoea or constipation. However, there are others who have an excellent diet, exercise regularly, are not overweight, and never strain when they go to the toilet, yet suffer from significant haemorrhoidal disease. Very little can be done to prevent haemorrhoids forming and progressing in these people.
Non-surgical
A colorectal surgeon has a wide variety of treatments available to treat haemorrhoidal disease. Some can be performed in the clinic and others can only be done in the operating theatre under general anaesthesia.
Injection sclerotherapy or rubber band ligation of haemorrhoids can be done in the clinic without anaesthesia. These procedures are only useful for internal haemorrhoids, where the aim of treatment is to reduce the blood supply. They cannot be used for external haemorrhoids as this would entail treating skin on the outside of the body, which would be extremely painful. Normal skin sensation stops half way up the back passage and above this bowel sensation starts. The bowel has a much lower capacity to sense pain than normal skin does. Therefore, injections or bands are suitable for haemorrhoids present above this sensory level. Patients do experience some sensation when these procedures are being performed, but it is not painful. The surgeon will check that normal skin sensation has ceased before injection sclerotherapy or rubber band ligation is started.
Overall, injections and banding seem to help in 70% of patients. They do not cure haemorrhoids, but can certainly reduce symptoms to a manageable level. It must be remembered that haemorrhoid tissue does have a positive role in the body.
Surgery
Surgical treatments for haemorrhoids need to be performed in the operating theatre. They are all performed as open procedures and are reserved for external and internal haemorrhoids that cannot treated by injection sclerotherapy or rubber band ligation.
If the problem is external haemorrhoids, a traditional haemorrhoidectomy is needed, where the haemorrhoidal tissue is removed and the wounds may be closed with dissolvable stitches. If the problem is internal haemorrhoids, a traditional haemorrhoidectomy may also be performed, but may be combined with Doppler-guided haemorrhoidal artery ligation (HAL) and/or rectoanal repair (RAR, also known as haemorrhoidopexy). Another surgical option for internal haemorrhoids is a stapled haemorrhoidopexy. People who have stapled surgery may have less postoperative pain than people who have the more traditional haemorrhoid surgery, but are slightly more likely to have their haemorrhoids come back and need surgery again.
For more information on haemorrhoids, please visit http://patient.info/health/piles-haemorrhoids.

