- Abscess Incision and Drainage
- Advancement Flap Repair
- Anal Bulking
- Anal Tattooing
- Botulinum Toxin Injection
- Colectomy
- Delorme’s Procedure
- ELAPE Procedure
- Femoral Hernia Repair
- Fistulotomy
- Haemorrhoidectomy
- HALO-RAR Procedure
- Inguinal Hernia Repair
- Intersphincteric APR
- Lateral Internal Sphincterotomy
- Low Anterior Resection
- Pelvic Organ Prolapse
- Perineal Rectosigmoidectomy
- Rectoanal Repair
- Rubber Band Ligation
- Stapled Haemorrhoidopexy
- Stoma Creation
- Stoma Reversal
- Transanal Rectocoele Repair
- Umbilical Hernia Repair
Inguinal Hernia Repair
Surgery is recommended for most adults who have symptoms from an inguinal hernia. The hernia is unlikely to get better by itself and the risk of complications increases with age. Repair of an inguinal hernia can be performed as an open orlaparoscopic (keyhole) procedure. There are a number of issues to consider when choosing between these two approaches which will be discussed thoroughly with you. For example, if you have had multiple abdominal operations before or have major ongoing medical problems, an open approach is generally needed. On the other hand, if you are otherwise fit and well and need to return to work as soon as possible, or have bilateral inguinal hernias (one on each side), the laparoscopic approach would be a better option.
You will have the opportunity to discuss fully all the risks and benefits of this operation with me before signing your consent form.
When performed using the traditional open approach (herniorrhaphy), a small 6–8 cm cut is made in the groin to access the hernia. The bulging (herniated) loop of bowel or fatty tissue is then returned to its correct place in the pelvic cavity. A special mesh* patch is then used to reinforce the abdominal wall, which reduces the risk of the hernia returning.
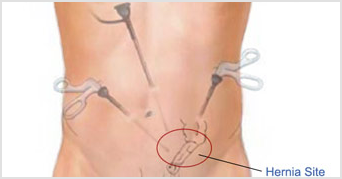
The laparoscopic approach for an inguinal hernia repair is similar to the open one except that the hernia is repaired with mesh using instruments inserted through small cuts on your abdomen.Three cuts (1–1.5 cm long) are made (one near the umbilicus and the others about 10 cm away on either side). A tube-like telescopic camera is inserted through one of the cuts so that the hernia can be seen on a television screen, and surgical instruments are passed through the other two cuts to repair the hernia. The mesh used in the laparoscopic procedure is larger than an open mesh repair and is secured in place by plastic tacks.
As a last step with both procedures, the wound(s) on the surface of the skin are closed with dissolvable stitches, followed by application of surgical glue that makes the wound watertight. Both procedures take about 30–60 minutes to perform.
Very occasionally (in less than 1% of cases) an inguinal hernia repair cannot be completed using the laparoscopic approach and we need to switch to an open approach.
Whether open or laparoscopic, an inguinal hernia repair is generally done as a day-stay procedure. A laparoscopic repair is always done under general anaesthesia, but an open repair can be done under either general or local anaesthesia.
If you have general anaesthesia you will be asleep and not feel any pain, and if you have local anaesthesia you will still feel no pain but will be awake during the procedure. Local anaesthesia needs multiple injections of local anaesthetic. The choice between these two types of anaesthesia depends on patient choice as long as the hernia repair is a technically simple one.
If you are having general anaesthesia, you will need to fast from midnight on the night before if your surgery is scheduled for the morning, or from 7 am if it is scheduled for the afternoon. No fasting is required if your procedure is to be performed under local anaesthesia.
The injection of local anaesthetic given in the operating theatre will help to keep you pain-free in the 6 hours following your surgery. After the operation you will be transferred to the recovery area and then to the ward. You should be able to go home the same day, but sometimes patients may need to stay longer. You should not drive after your surgery, so a friend or relative will need to take you home.
Pain is common after a hernia repair when your local anaesthetic wears off. The pain often takes up to 4 weeks to resolve completely. Analgesic medication will be given to you to take home. Some types of analgesia cause constipation so you will be given laxatives to take home as well.
The watertight surgical glue applied to your wound site(s) sets in 3 minutes so you can bathe and shower as normal when you get home. The glue can be picked off at home 10 days after your surgery.
When you can resume life as normal depends mainly on your home circumstances and/or the type of job you have, and this will be discussed with you in detail in clinic well before your operation date. You can return to work when you have been cleared to do so. Whether you have had an open or laparoscopic mesh repair, normal activity can be resumed once postoperative pain allows. In general, most people are able to return to their normal activity levels within 4 weeks of surgery.
Inguinal hernias are much more common in men than in women. Unfortunately, repair of this type of hernia is more difficult in men because of the important structures that are in close contact with the herniated tissue in men, ie, the spermatic cord and nerves and blood vessels supplying the male reproductive organs. Fortunately, complications arising from damage to these structures during an inguinal repair are rare, but even with perfect surgery complications can occur.
Throughout the world, there is an up to 3 in 100 chance of being left with long-term pain after inguinal hernia surgery. Nothing has gone wrong with the operation. Unfortunately, the healing process may result in the nerves in the area being involved in the scar tissue. The chances of this type of long-term pain seems to be less with keyhole surgery and if the type of synthetic mesh used is chosen wisely. This is a nerve-type pain, which is very different from normal pain. Nerve pain is difficult to manage and in some people they are so limited by the pain that it may prevent them from returning to work. However, as with all surgery, the risks of an operation must be balanced against the risks of not operating. The risks of leaving a hernia alone include a 1 in 100 chance of needing emergency surgery for an obstructed hernia each year, and the risks that entails.
Exactly when patients can resume driving after this type of surgery is determined on a case-by-case basis. This is usually 2 weeks, but will be discussed with you after your surgery. Please let your insurance company know when you have been given the all-clear to resume driving.
In the unlucky event that an inguinal hernia become trapped (strangulated) and part of the bowel is damaged, the affected part may need to be removed and the two ends of healthy bowel rejoined. This is a bigger operation done as an emergency, and you may need to stay in hospital for 4–5 days to allow the injured area of the bowel to settle.
A follow-up appointment in the clinic will be arranged in 1–2 weeks after your surgery to check your wound(s) and discuss any further management if required.
*Surgical mesh has been the subject of much media coverage in the news. However, there is a lot of confusion around this. The mesh products associated with failed procedures and increased rates of infection were materials that were poorly designed and poorly engineered, and were used by some surgeons in the pelvis when they were not intended for this type of surgery. I do not use these meshes in colorectal surgery. I use synthetic meshes and to a lesser degree biological meshes. A synthetic mesh is a sterile woven material made of plastic. This type of mesh does not dissolve, and the specific type of synthetic mesh used needs to be carefully chosen for each use looking at multiple aspects of the mesh itself. The correct use of synthetic mesh results in a very low risk of infection, and has been used safely in the treatment of hernias for decades.

