- Abscess Incision and Drainage
- Advancement Flap Repair
- Anal Bulking
- Anal Tattooing
- Botulinum Toxin Injection
- Colectomy
- Delorme’s Procedure
- ELAPE Procedure
- Femoral Hernia Repair
- Fistulotomy
- Haemorrhoidectomy
- HALO-RAR Procedure
- Inguinal Hernia Repair
- Intersphincteric APR
- Lateral Internal Sphincterotomy
- Low Anterior Resection
- Pelvic Organ Prolapse
- Perineal Rectosigmoidectomy
- Rectoanal Repair
- Rubber Band Ligation
- Stapled Haemorrhoidopexy
- Stoma Creation
- Stoma Reversal
- Transanal Rectocoele Repair
- Umbilical Hernia Repair
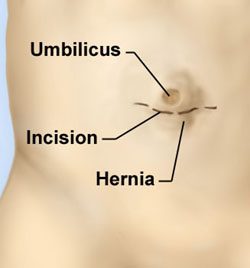
Umbilical Hernia Repair
Surgery is recommended for most adults who have symptoms from an umbilical hernia. The hernia is unlikely to get better by itself and the risk of complications increases with time. Repair of an umbilical hernia can be performed as an open or laparoscopic (keyhole) procedure. There are a number of issues to consider when choosing between these two approaches which will be discussed thoroughly with you. For example, if you have had multiple abdominal operations before or have major ongoing medical problems, an open approach is generally needed. On the other hand, if you are otherwise fit and well and need to return to work as soon as possible, the laparoscopic approach could be a better option.
You will have the opportunity to discuss fully all the risks and benefits of this operation with me before signing your consent form.
When performed using the traditional open approach (herniorrhaphy), a small 2–3 cm cut is made just above or below the navel to access the hernia. The bulging (herniated) loop of bowel or abdominal fat is then returned to its correct place in the abdominal cavity. For small umbilical hernias (less than 1 cm), the opening in the abdominal wall is closed by stitching the muscle layers together; for larger hernias, a special mesh* patch is used to reinforce the abdominal wall, which reduces the risk of the hernia returning.
The laparoscopic approach for an umbilical hernia repair is similar to the open one except that the hernia is repaired with mesh using instruments inserted through small cuts in the left lower part of your abdomen. Three cuts (1–1.5 cm long) are made: a tube-like telescopic camera is inserted through one of the cuts so that the hernia can be seen on a television screen, and surgical instruments are passed through the other two cuts to repair the hernia. The mesh used in the laparoscopic procedure is larger than for an open mesh repair and is secured in place by plastic tacks. The area of tacking is larger than the securing needed in open surgery, so immediate postoperative pain is understandably more.
As a last step with both procedures, the wound(s) on the surface of the skin are closed with dissolvable stitches, followed by application of surgical glue that makes the wound watertight. Both procedures take about 30 minutes to perform.
Very occasionally (in less than 1% of cases) an umbilical hernia repair cannot be completed using the laparoscopic approach and we need to switch to an open approach.
Whether open or laparoscopic, an umbilical hernia repair is generally done as a day-stay procedure under general anaesthesia, so you will be asleep and not feel any pain. You will need to fast from midnight on the night before if your surgery is scheduled for the morning, or from 7 am if it scheduled for the afternoon.
You will be given an injection of local anaesthetic before you leave the operating theatre to help keep you pain-free in the 6 hours after your surgery. After the operation you will be transferred to the recovery area and then to the ward. You should be able to go home the same day, but sometimes patients may need to stay longer. You should not drive after your surgery, so a friend or relative will need to take you home.
Pain is common after a hernia repair when your local anaesthetic wears off. The pain may take up to 4 weeks to resolve completely. Analgesic medication will be given to you to take home.
The watertight surgical glue applied to your wound site(s) sets in 3 minutes so you can bathe and shower as normal when you get home. The glue can be picked off at home 10 days after your surgery.
Exactly when you can resume life as normal depends mainly on your home circumstances and/or the type of job you have, and this will be discussed with you in some detail in clinic well ahead of your scheduled surgery. You can return to work when you have been cleared to do so. With the simple suture repair, people should avoid heavy lifting and strenuous activities for 4 weeks. As a general guide, it is safest not to lift anything heavier than a full kitchen jug of water during this time. For both open and laparoscopic mesh repair, strenuous activities can be resumed once postoperative pain allows. In general, most people are able to return to their normal activities within 4 weeks of surgery. However, some people do take longer.
Exactly when patients can resume driving after this type of surgery is determined on a case-by-case basis. This is usually 2 weeks, but will be discussed with you after your surgery. Please let your insurance company know when you have been given the all-clear to resume driving.
In the unlucky event that an umbilical hernia become trapped (strangulated) and part of the bowel is damaged, the affected part may need to be removed and the two ends of healthy bowel rejoined. This is a bigger operation done as an emergency, and you may need to stay in hospital for 4–5 days to allow the injured area of bowel to settle. This is usually done as an open procedure, but sometimes it may be done laparoscopically if possible.
A follow-up appointment in the clinic will be arranged in 1–2 weeks after your surgery to check your wound(s) and discuss any further management if required.
*Surgical mesh has been the subject of much media coverage in the news. However, there is a lot of confusion around this. The mesh products associated with failed procedures and increased rates of infection were materials that were poorly designed and poorly engineered, and were used by some surgeons in the pelvis when they were not intended for this type of surgery. I do not use these meshes in colorectal surgery. I use synthetic meshes and to a lesser degree biological meshes. A synthetic mesh is a sterile woven material made of plastic. This type of mesh does not dissolve, and the specific type of synthetic mesh used needs to be carefully chosen for each use looking at multiple aspects of the mesh itself. The correct use of synthetic mesh results in a very low risk of infection, and has been used safely in the treatment of hernias for decades.

